Diagnosing heart failure using the correct pathway
LOUISE CLAYTON
LOUISE CLAYTON
Advanced Nurse Practitioner, University Hospitals of Leicester NHS Trust, Co-chair Alliance for Heart Failure
Practice Nurse 2022;52(7):22-23
In our previous article we looked at how to recognise and monitor the symptoms of heart failure in primary care. In the second article in this series from the Alliance for Heart Failure we will look at how to formally diagnose a suspected case and refer to a specialist
Some 40% of patients who receive their diagnosis in hospital had symptoms that could have triggered an earlier assessment in primary care.1,2 Therefore, knowing how to put patients on the correct pathway can dramatically improve their long term prognosis, reduce hospitalisations and even save lives.2
THE NT-proBNP TEST – ASSESSING THE RESULTS
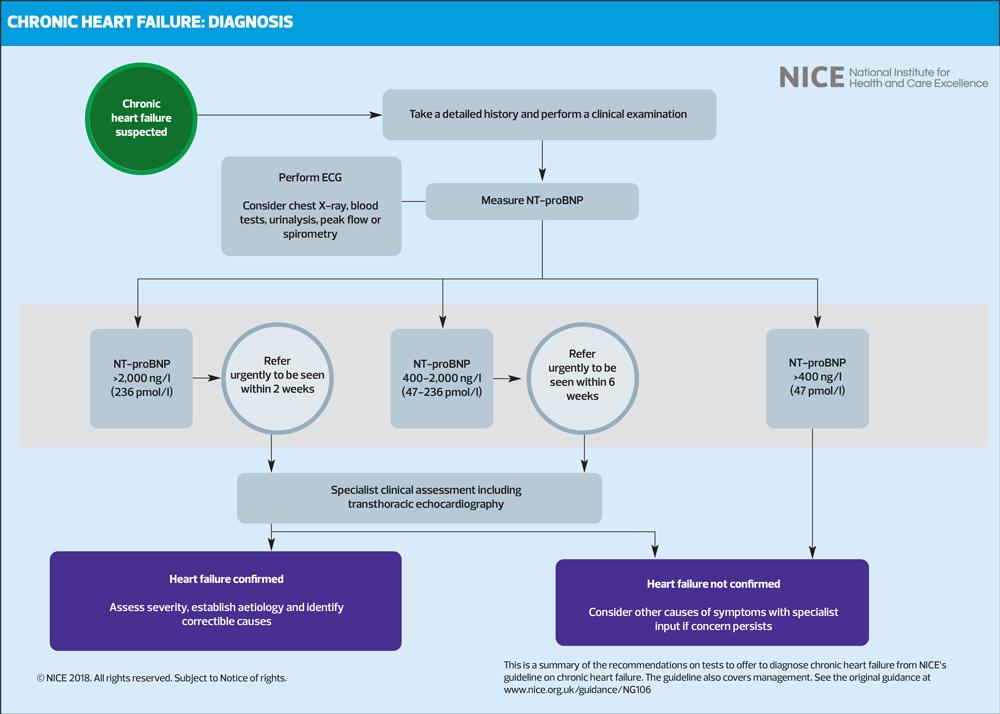
At the end of the first article, we looked at how an NT-proBNP test can be used to confirm a suspected case of heart failure. The results of this test can determine how urgent a referral should be.
An NT-proBNP level above 2000ng/litre needs to be urgently referred for specialist assessment and echocardiography (echo) within two weeks.3
Those with a level between 400 and 2000ng/litre should be referred within six weeks.3
However, your own judgement can play a part when assessing how quickly to refer. If a patient presents closer to the 2000 mark, there is nothing stopping you from making a holistic risk assessment using the patient’s symptoms, age and comorbidities when referring.
A level below 400 makes a heart failure case less likely but does not necessarily rule it out. You should consider other causes of breathlessness before ruling out heart failure, and seek specialist input if concerns persist.3
REFERRAL FOLLOWING A POSITIVE NT-proBNP TEST
Once you have the NT-proBNP test result you can refer the patient for an echocardiogram. This is a specialist service that takes place at a hospital or community diagnostic centre.
Access to echocardiography services can vary depending on your area. Some practices may have access to community echocardiographic clinics while others may require a patient to be referred to a nearby hospital. If you haven’t already, familiarise yourself with your local heart failure specialist through your GP. This will give you an idea of what’s available and where.
While waiting for an echo result, you should liaise with a specialist for advice and guidance on how to start treatment in primary care. This is important for ensuring there is no unnecessary delay to any treatment. This will be covered in more detail in our next article.
COMMUNICATING YOUR REFERRAL TO THE PATIENT
Specialist referral for patients with heart failure symptoms can be alarming. It is important to communicate your concern in relation to their specific symptoms and medical history. The phrase ‘heart failure’ can sound alarming, and while you should be honest and frank about your suspected diagnosis, you should reassure the patient that they are on course to receive the best possible care.
While a patient is waiting for a referral, you should encourage them to closely monitor and report any worsening symptoms.
WHAT NEXT?
In our next article we look at how general practice nurses can treat heart failure in primary care.
REFERENCES
1. Conrad N, Judge A, Canoy D, et al. Diagnostic tests, drug prescriptions, and follow-up patterns after incident heart failure: A cohort study of 93,000 UK patients. PLOS Medicine. 2019;16(5)
2. Bottle A, Kim D, Aylin P, et al. Routes to diagnosis of heart failure: observational study using linked data in England. Heart 2018; 104(7):600-5.
3. NICE NG106. Chronic heart failure in adults: diagnosis and management; 2018. https://www.nice.org.uk/guidance/ng106
Related articles
View all Articles