Diagnosing and monitoring heart failure
In association with the Alliance for Heart Failure
In association with the Alliance for Heart Failure
Practice Nurse 2022;52(6):22-23
As the NHS emerges from the pandemic, we will once more have to face up to the huge and ever-growing burden of heart failure. Nearly a million people currently live with the condition,1 with hospital admissions set to rise by 50% in the next 25 years.2 Part 1: Recognising the key symptoms of heart failure and what to do next
Primary care has a major part to play in tackling the increasing burden of heart failure, with GPs and general practice nurses playing a vital role in both early diagnosis and the long term management of the condition in the community.
This year, the Alliance for Heart Failure is calling on general practice nurses to help tackle the ever-growing burden of heart failure. In this series of three articles, we aim to help you recognise the key symptoms, diagnose using the correct pathways and provide the best possible treatment in primary care.
DIAGNOSING AND MONITORING HEART FAILURE
General practice nurses are on the frontline when it comes to spotting heart failure cases. Daily, they come into contact with high risk patients.
Heart failure is the leading cause of hospital admissions in the over 65s and has high prevalence among those attending for regular review for long term illnesses such as diabetes, hypertension and chronic kidney disease.3
However, heart failure is also a complex clinical syndrome that has a variety of different causes, with symptoms that are often confused for long term conditions such as asthma or other chronic respiratory conditions.
Due to this, opportunities for early diagnosis are often missed in primary care. Less than 10% of patients receive their heart failure diagnosis from their GP practice, with most cases being diagnosed in hospital.4
Knowing signs of worsening heart failure can also help monitor the disease among existing patients. Therefore, being proactive, vigilant and curious about the signs and symptoms of heart failure can prevent hospitalisation in new cases and allow you to better manage those living with heart failure.
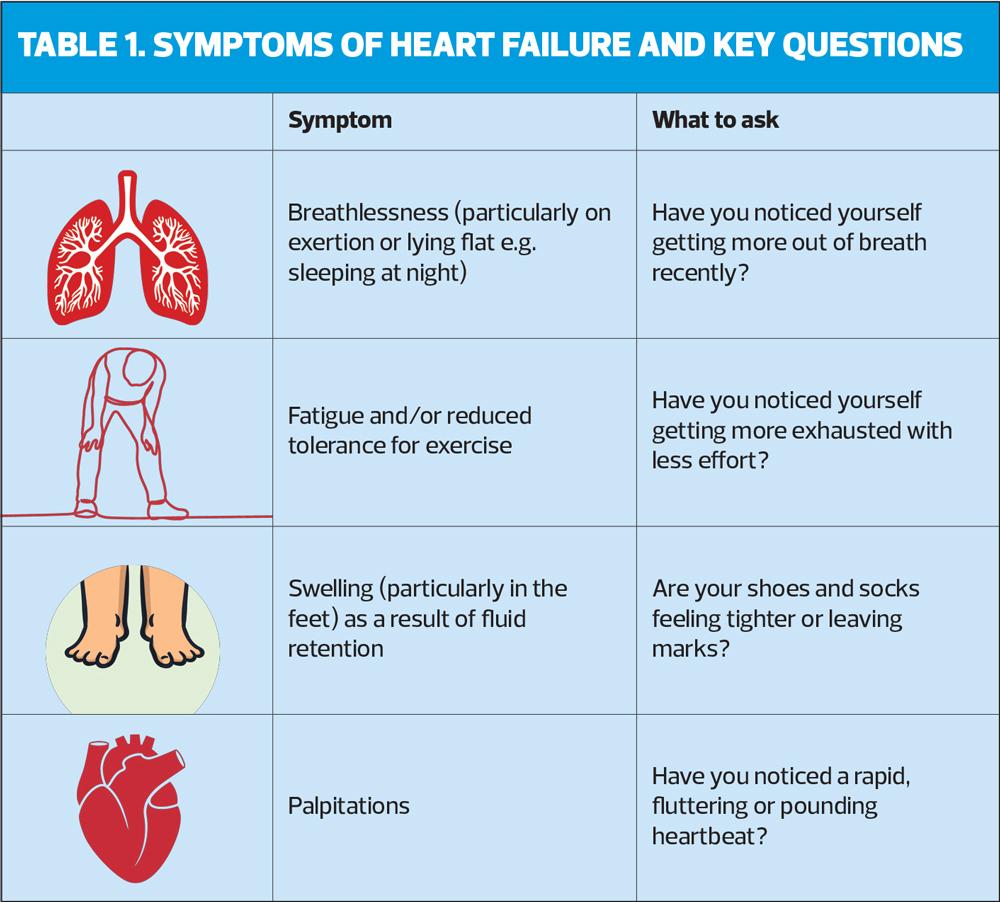
SYMPTOMS, WARNING SIGNS AND WHAT TO ASK
Heart failure symptoms can be of rapid onset or develop more gradually over a long-term period.
Someone with chronic heart failure also may have episodes of decompensation where their symptom burden increases.
Some simple questions during a consultation can help to identify any issues (Table 1).
Also consider comorbidities when it comes to diagnosing heart disease:
- Nearly a third of patients admitted to hospital for heart failure have diabetes5
- Just under 20% have chronic obstructive pulmonary disease (COPD)5
- Having a family history of heart failure, or heart problems, particularly cardiomyopathy, raises the risk.
Heart failure is most commonly misdiagnosed as anxiety, asthma, stress and chest infections. If you suspect a case, you should act.
Maintaining a register of patients is the first indicator on the QOF (Quality and Outcomes Framework) for heart failure. If your surgery doesn’t have one, you should discuss with your lead practitioner its benefits when it comes to monitoring heart failure patients, particularly those with comorbidities.
WHAT TO DO IF YOU SUSPECT HEART FAILURE?
Where heart failure is suspected, a patient can be sent for a NT-proBNP test. This is a simple test that can measure the level of natriuretic peptides in the blood, a biological marker for the severity of heart disease.
Practice nurses can request a NT-proBNP test and perform it themselves in surgery. A 2020 survey estimated that in England around 72% of trusts in primary care had access to NT-proBNP tests.1 If you do not have access to one, you should discuss it with your GP.
WHAT NEXT?
In the next two articles, we will explain how practice nurses can use the results of these tests to accurately diagnose a new or worsening case of heart failure and provide patients with the best possible care.
REFERENCES
1. British Heart Foundation (BHF). UK Factsheet January 2020. https://www.bhf.org.uk/what-we-do/our-research/heart-statistics
2. NICE CG106. Chronic heart failure in adults: diagnosis and management; September 2018. https://www.nice.org.uk/guidance/ng106
3. NICE CG187. Acute heart failure: diagnosis and management; October 2014. https://www.nice.org.uk/guidance/cg187
4. Heart failure: The hidden costs of late diagnosis. Census wide data from a survey of 625 heart failure patients in 2020. Roche Diagnostics Limited, Pumping Marvellous; 2020
5. Kahn MS, Tahhan AS, Vaduganathan M. Trends in prevalence of comorbidities in heart failure clinical trials. Eur J Heart Failure 2020;22:1032-1042. https://doi.org/10.1002/ejhf.1818
Related articles
View all Articles