Stop smoking interventions and services. NICE NG92, March 2018
May 2018
May 2018
Guidance from NICE aims to ensure that everyone who smokes is advised and encouraged to stop and given the support they need. It emphasises the importance of targeting vulnerable groups who find smoking cessation hard or who smoke a lot. The guidance is aimed not only at those responsible for commissioning services but healthcare professionals delivering stop smoking interventions in primary and community care settings.
Note: this guidance has been updated. See NG209, https://www.nice.org.uk/guidance/ng209
NICE wants to see evidence-based interventions and services are provided for everyone who smokes, especially those in priority groups.
The priority groups are those people who are at high risk of tobacco-related harm, including:
- People with mental health problems, including mental health disorders
- People who misuse substances
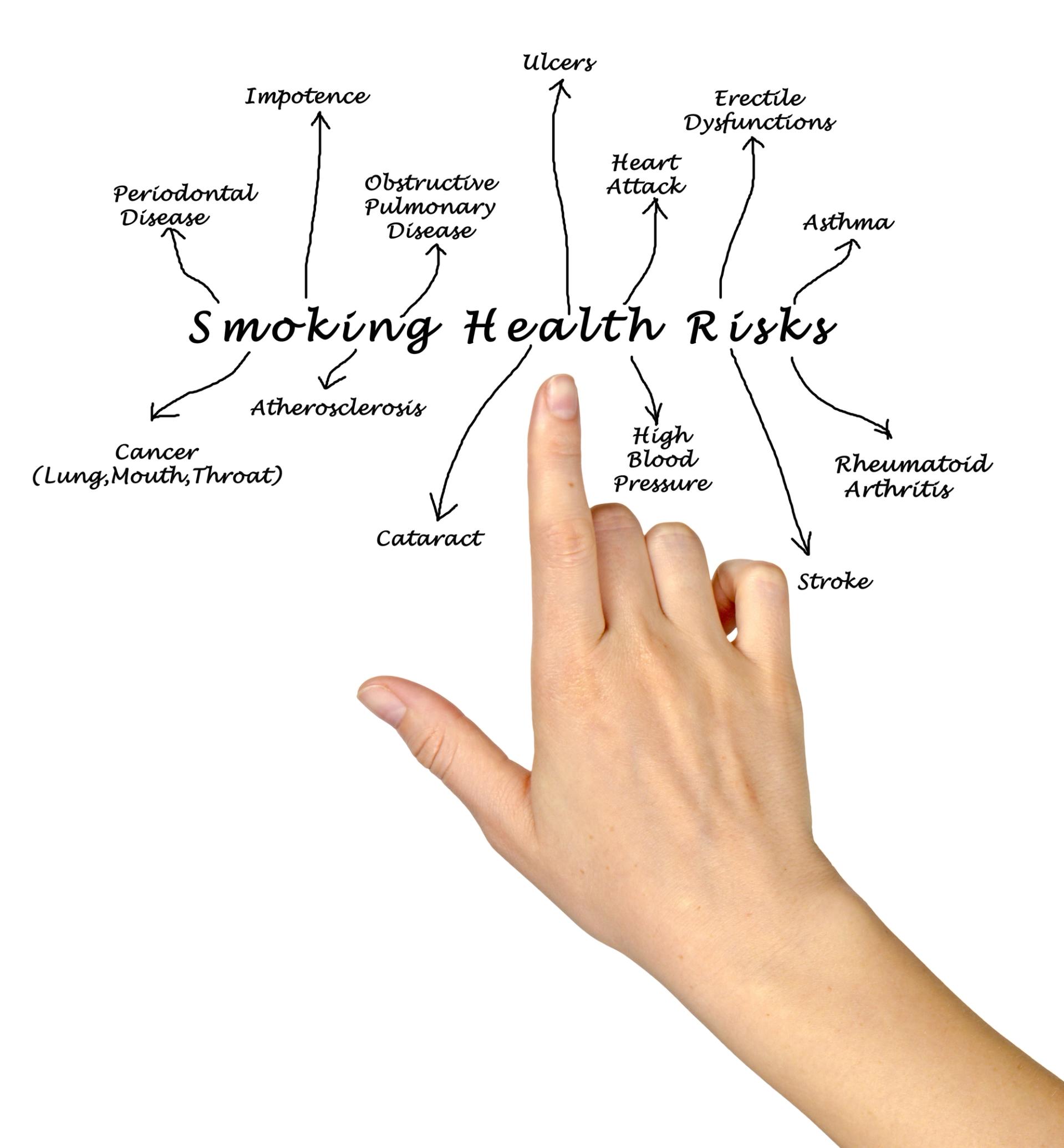
- People with health conditions caused or made worse by smoking (including cardiovascular disease – especially those most at risk of dying early, type 1 diabetes, asthma and COPD)
- People with a smoking-related illness e.g. lung cancer
- Populations with a high prevalence of smoking-related morbidity or high susceptibility to harm
- Communities or groups with particularly high smoking prevalence (such as manual workers, travellers, LGBT people)
- People in custodial settings
- People living in disadvantaged circumstances
- Pregnant women who smoke
The aim should be to treat at least 5% of the estimated local population who smoke each year, with a target quit rate of at least 35% at 4 weeks.
The evidence-based interventions that should be available for adults who smoke include:
- Behavioural support
- Bupropion
- Nicotine replacement therapy (NRT) – short and long acting
- Varencline
- Very brief advice (Ask about current and past smoking, provide information on the consequences of smoking and stopping smoking, and advise on options for support and pharmacotherapy – see the NCSCT Very Brief Advice training module, at http://www.ncsct.co.uk/publication_very-brief-advice.php )
ENGAGING WITH PEOPLE WHO SMOKE
At every opportunity, ask people if they smoke and advise them to stop smoking in a way that is sensitive to their preferences and needs.
Encourage people who are being referred for elective surgery to stop smoking before their surgery. Refer them to local stop smoking support.
Discuss any stop smoking aids the person has used before, including personally purchased nicotine-containing products.
Offer advice on using nicotine-containing products on general sale, including NRT and nicotine-containing e-cigarettes.
- Nicotine-containing e-cigarettes are not licensed medicines but they are regulated
- Many people have found them helpful to quit smoking cigarettes
- People using e-cigarettes should stop smoking tobacco completely, because any smoking is harmful
- The evidence suggests that e-cigarettes are substantially less harmful to health than smoking but are not risk free
EVIDENCE-BASED STOP SMOKING INTERVENTIONS
For adults, prescribe varencline, bupropion or NRT before they stop smoking (varencline should normally only be offered as part of a programme of behavioural support).
Agree a quit date set within the first 2 weeks of buproprion treatment and within the first 1 – 2 weeks of varencline treatment. The smoker should be reassessed shortly before the prescription ends.
Agree a quit date if NRT is prescribed, and ensure that the smoker has NRT ready to start the day before the quit date.
Consider NRT for young people over 12 who are smoking and dependent on nicotine. If prescribed, it should be offered with behavioural support.
IF A SMOKER WANTS TO QUIT
- Refer to local stop smoking support services
- Discuss how to stop smoking (access NCSCT online training at http://elearning.ncsct.co.uk )
- Discuss the pharmacotherapy and behavioural options available
- Explain that a combination of varencline and behavioural support OR a combination of short- and long-acting NRT are likely to be most effective
- Agree the approach to stopping smoking that best suits the individual’s preferences
IF A SMOKER IS NOT READY TO QUIT
- Make sure they understand that stopping smoking reduces the risk of developing smoking-related illnesses or worsening conditions affected by smoking
- Ask them to think about harm reduction – see Smoking: harm reduction [PH45] https://www.nice.org.uk/guidance/ph45
- Encourage them to seek help to quit smoking completely in the future
- Record the fact that they smoke and ask about it again at every opportunity in a way that is sensitive to their preferences and needs
RESOURCES
NICE NG209. Tobacco: preventing uptake, promoting quitting and treating dependence; 2021, updated 2025. https://www.nice.org.uk/guidance/ng209
National Centre for Smoking Cessation and Training (NCSCT) Very Brief Advice training module. http://www.ncsct.co.uk/publication_very-brief-advice.php
NCSCT Online training http://elearning.ncsct.co.ukNICE PH45. Smoking: harm reduction, 2013. https://www.nice.org.uk/guidance/ph45
PRACTICE NURSE FEATURED ARTICLES
e-cigarettes – a potential game-changer in getting people to stop smoking Mandy Galloway
Tobacco: Reducing the harm Dr Ed Warren
Smoking cessation: Tailoring your approach to the individual smoker Darush Attar-Zadeh
Reference
NICE NG92. Stop smoking interventions and services, March 2018 https://www.nice.org.uk/guidance/ng92
Related guidelines
View all Guidelines