Practice nurse bite-sized learning: Understanding resistant hypertension
Joanne Haws, Michaela Nuttall
Joanne Haws
RN MSc
Clinical Director, Learn With Nurses
Michaela Nuttall
RGN MSc
Founder & Director, Learn With Nurses
Michaela Nuttall
RGN MSc
Founder & Director, Learn With Nurses
Practice Nurse 2025;55(2):7-8
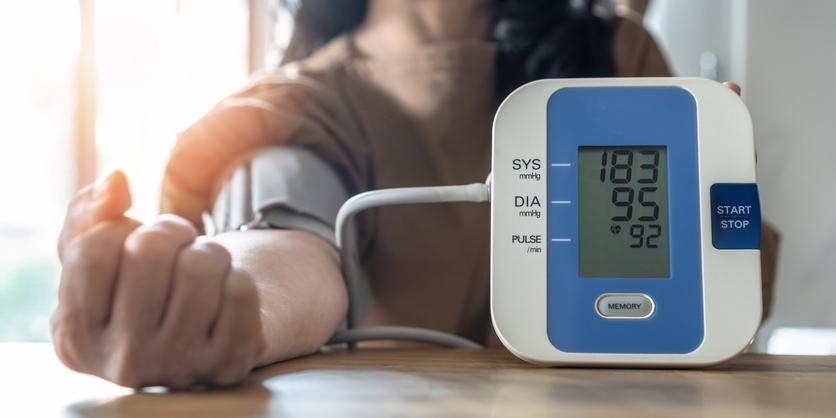
Almost a third of adults in the United Kingdom have persistently high blood pressure (hypertension), and at least a third of these have not managed to achieve blood pressure targets despite treatments. Although treatment in some cases is suboptimal, a proportion of these individuals will have resistant hypertension (RH).1
WHAT’S THE PROBLEM?
Hypertension is the third biggest risk factor for premature deaths and disability after smoking and poor diet, with at least half of all hearts attacks and strokes being associated with high blood pressure.1 Individuals with uncontrolled blood pressure have a 50% greater risk of cardiovascular and kidney disease compared with those who achieve target levels.2
DIAGNOSIS
NICE defines RH as blood pressure that remains uncontrolled despite taking optimal tolerated doses of an angiotensin converting enzyme inhibitor (ACEi) or angiotensin receptor blocker (ARB) in combination with a calcium channel blocker (CCB) and a thiazide-type diuretic.3 It is really important to exclude inaccurate measurement and non-adherence to therapies to avoid an incorrect diagnosis and further prescribing. Confirmation of clinic blood pressure readings of ≤140/90 mmHg and a daytime average (using ambulatory or home blood pressure measurement) of ≤135/85 mmHg should be made, alongside an assessment of adherence to medication before a diagnosis of RH is made.
MANAGEMENT
There is much that can be offered in a non-specialist setting to support individuals with RH, starting with a review of modifiable risk factors. Obesity, salt intake, physical inactivity and excessive alcohol are all independently associated with RH and management of these factors is recommended in all national and international guidance.1 See Table 1
It is also useful to discuss, review, and avoid where possible, potential hypertension-inducing medication use including the use of hormone and steroid therapies, as well as over the counter products such as non-steroidal anti-inflammatory drugs and decongestants.
If further anti-hypertensive prescribing is indicated, the addition of the mineralocorticoid receptor antagonist (MRA) spironolactone 12.5–25mg once daily is recommended as a fourth line agent. Renal function and potassium (K+) levels should be closely monitored with eGFR > 30 mL/min/1.73m2 and K+ < 4.5 mmol/L confirmed before initiation (Table 2).
REFERRAL
Where achievement of BP target (Table 3) is still not attained despite optimising both pharmacological and non-pharmacological approaches referral to a hypertension specialist should be considered. This will allow for further assessment of potential causes of secondary hypertension, objective assessment of treatment adherence and further management as required.
REFERENCES
1. Faconti L, George J, Partridge S, et al. Investigation and management of resistant hypertension: British and Irish Hypertension Society position statement. J Hum Hyperten 2025;39:1-14
2. NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37–55.
3. NICE NG136. Hypertension in adults: diagnosis and management; 2022. https://www.nice.org.uk/guidance/ng136
4. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289(19):2560–2571.
Related articles
View all Articles
